Jakub Podolec, Jakub Baran, Łukasz Niewiara, Piotr Odrowąż-Pieniążek, Krzysztof Żmudka
Department of Interventional Cardiology, Medical College Jagiellonian University and the John Paul II Hospital, Krakow, Poland
Adv Interv Cardiol 2017; 13, 1 (47): 88–89
DOI: https://doi.org/10.5114/aic.2017.66196
Patients with stable coronary artery disease and diffuse long lesions are becoming more often a challenge for interventional cardiologists. Complete revascularization often requires implantation of many stents into a single artery. Overlapping of stents, required for drug-eluting stents (DES), leads to higher metal density, which is also potentially more favorable for healing problems and cardiac events [1–3].
A 62-year-old patient with hypertension, diabetes and dyslipidemia presented to the Department of Interventional Cardiology, Jagiellonian University College of Medicine in the John Paul II Hospital with moderate to severe angina (class II/III according to the Canadian Cardiovascular Society Classification), diagnosed 2 months ago with coronary artery disease. According to Heart
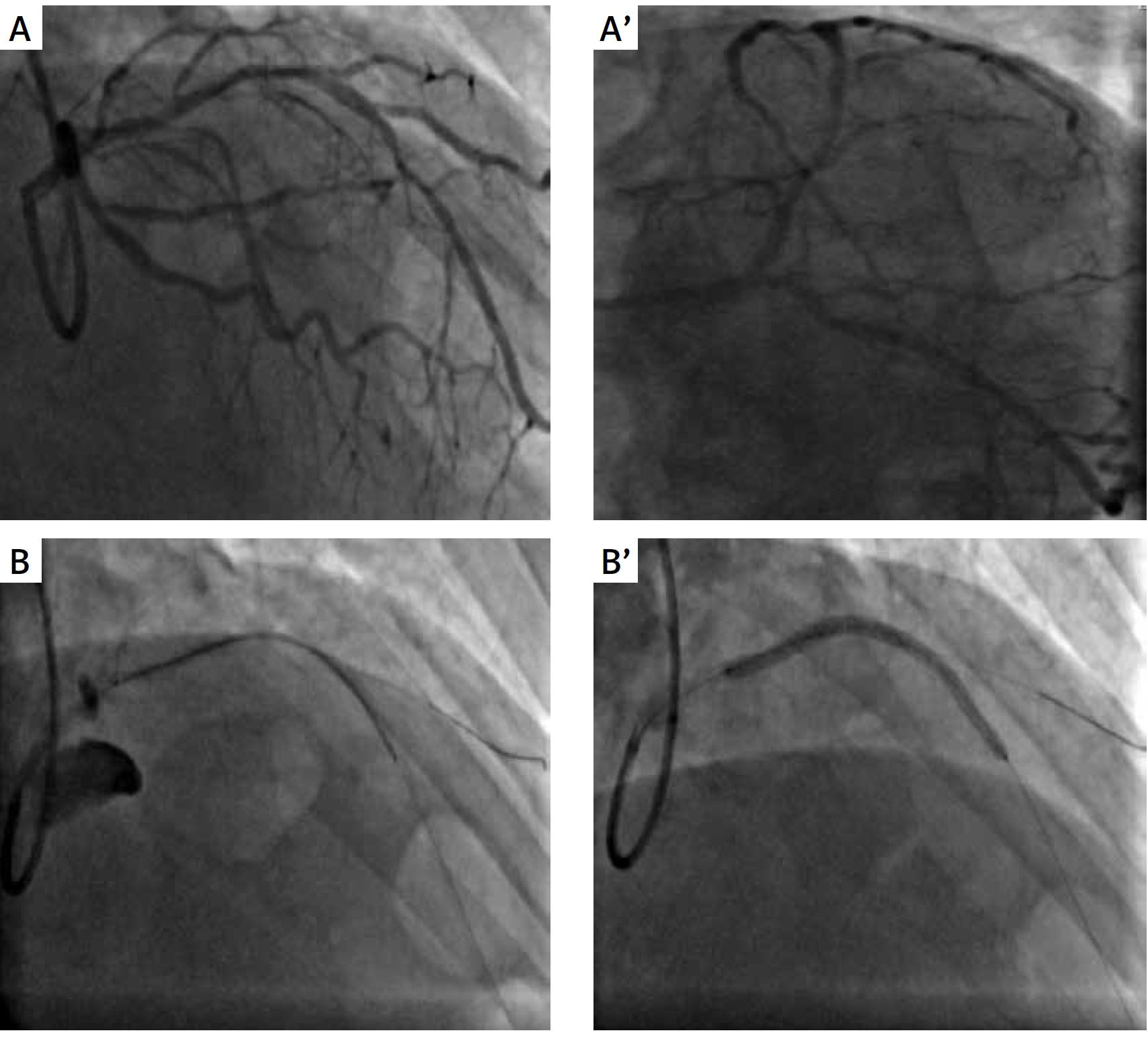
Team qualification, the patient was admitted to a referral invasive cardiology center to perform left anterior descending (LAD) angioplasty (Figure 1). The fractional flow reserve (FFR) result of 0.6 confirmed severity of the stenosis. Coronary angiography was performed and revealed a long calcified lesion in the proximal and mid segment of the LAD. Both the LAD and the diagonal (Dg) branch were secured with guide wires. To estimate the vessel diameter intravascular ultrasound (IVUS) was performed, but due to extensive arterial calcification in the proximal segment introduction of the Eagle eye IVUS catheter was impossible (Figure 1). Predilatation with a non-compliant balloon 3.0/15 mm up to 24 atm in the proximal and mid part was performed. Vessel diameter estimation after IVUS measurements was performed and revealed dissection in the mid part of the LAD. A 60 mm Sirolimus drug-eluting tapered Biomime morph stent with the proximal diameter of 3.0 and distal diameter of 2.5 mm was implanted without complications. The guidewire from the Dg branch was again introduced through the struts of the stent. The IVUS imaging showed a need of postdilatation in the mid part of the stent. Non-compliant 3.75/15 mm was used for optimization of the result. Kissing balloon technique was used to optimize the bifurcation result. The IVUS of the LAD also revealed non-critical distal dissection distally to the stent with slower blood flow to the distal part of the artery. A short 2.5/18 mm DES was implanted to cover the whole dissection distally. Final IVUS measurements revealed minimal lumen diameter (MLA) in the proximal part of the stent of 8.0 mm² and in the distal part 3.8 mm².
Proximally the plaque edge burden was 45.5%, and distally 52.8%. The IVUS measurements confirmed the good angiographic result.
The stent introduction after optimal lesion preparation with a non-compliant balloon was easy and predictable. Treatment of long lesions with single stent implantation is an interesting option for most patients and reduces the need for implantation of many overlapping stents.
Conflict of interest
The authors declare no conflict of interest.
References
1. Räber L, Jüni P, Löffel L, et al. Impact of stent overlap on angiographic and long-term clinical outcome in patients undergoing drug-eluting stent implantation. J Am Coll Cardiol 2010; 55:
1178-88.
2. O’Sullivan CJ, Stefanini GG, Räber L, et al. Impact of stent overlap on long-term clinical outcomes in patients treated with newer-generation drug-eluting stents. Eurointervention 2014; 9:
1076-84.
3. Colombo A, Al-lamee R. Interventional cardiology: does stent overlap make a difference to clinical outcome? Nature Rev Cardiol 2010; 7: 362-4.
Jakub Podolec et al. IVUS-guided implantation of a long, tapered DES Advances in
Corresponding author:
Jakub Baran, Department of Interventional Cardiology, Medical College Jagiellonian University and the John Paul II Hospital, 80 Pradnicka St, 31-202 Krakow, Poland, phone: +48 791 330 302, e-mail: jakub_baran@yahoo.pl Received: 26.10.2016, accepted: 19.02.2017.
Advances in Interventional Cardiology 2017; 13, 1 (47)